Alzheimer’s disease has long been considered a progressive and irreversible neurodegenerative disorder, marked by steady memory loss and cognitive decline. Despite decades of research, existing treatments have largely focused on slowing disease progression rather than repairing damage already done. That understanding may now be shifting.
A recent scientific study has reported Alzheimer’s reversal in mice, demonstrating that memory and cognitive function can be restored by correcting a fundamental metabolic failure in the brain. The findings suggest that neuronal dysfunction in Alzheimer’s may not be permanent and could be reversible under specific biological conditions.
While the research is limited to animal models, it introduces a new therapeutic direction that moves beyond traditional plaque-centric approaches and focuses instead on restoring cellular energy balance.
Table of Contents
Alzheimer’s Disease and the Long-Held Assumption of Irreversibility
Alzheimer’s disease is characterized by the gradual deterioration of neurons in brain regions responsible for memory, learning, and reasoning. Pathologically, the disease is associated with abnormal accumulation of amyloid-beta plaques and tau protein tangles, alongside chronic inflammation and synaptic loss.
For more than a century, these structural changes were believed to represent permanent damage. Once neurons were impaired or lost, recovery was considered biologically impossible. As a result, drug development efforts primarily aimed to delay disease progression rather than restore function.
The report of Alzheimer’s reversal in mice directly challenges this foundational assumption.
Related: Drug-Resistant Fungus Candida auris Spreading Worldwide
What the New Study Demonstrated
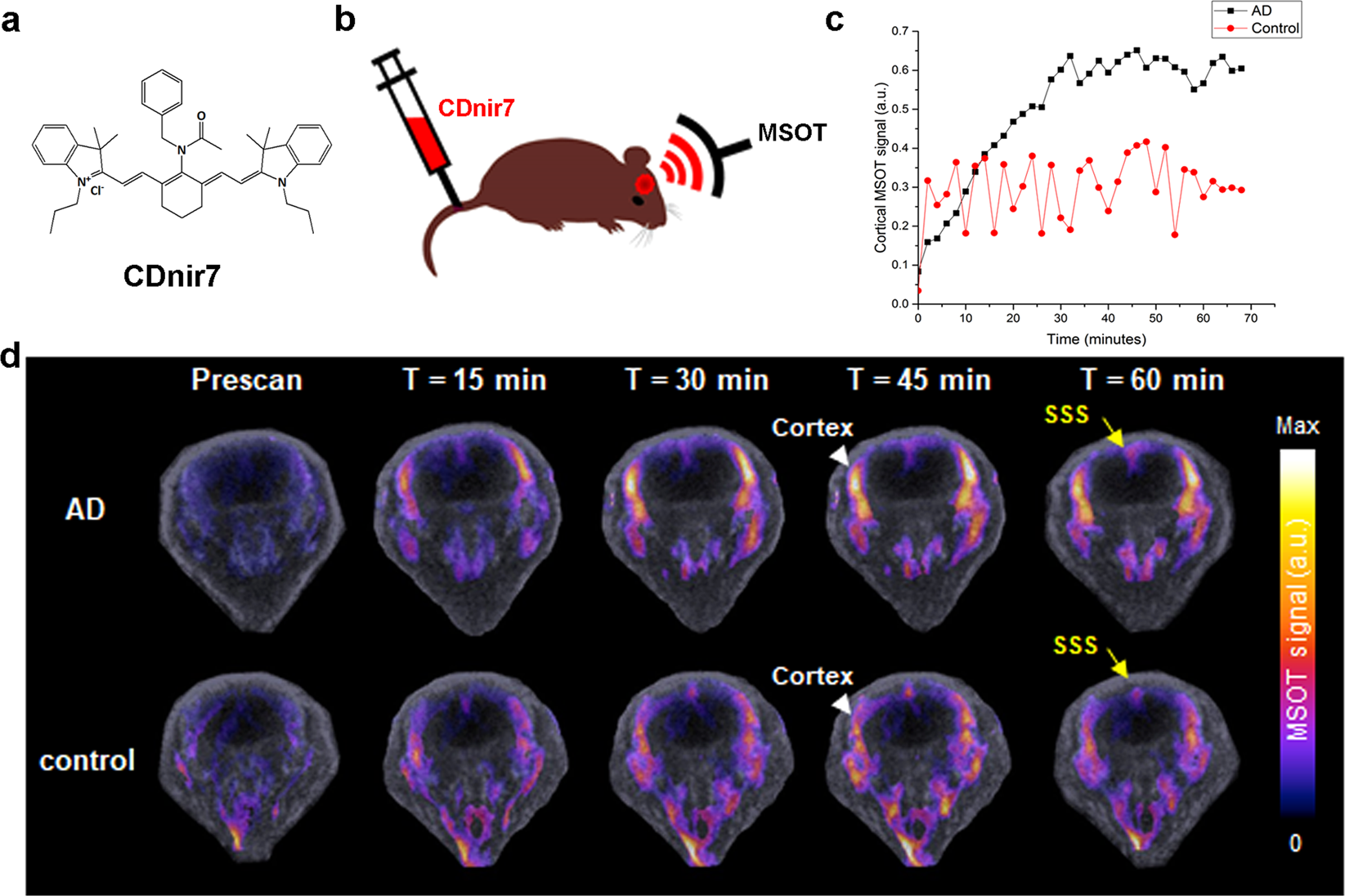
In the newly published research, scientists used a well-validated mouse model that develops Alzheimer’s-like pathology, including memory impairment and molecular hallmarks of the disease.
After intervention, researchers observed:
- Restoration of learning and memory performance
- Normalization of Alzheimer’s-associated blood biomarkers
- Recovery of neuronal metabolic function
Crucially, these improvements occurred even when treatment began after cognitive decline was already evident, a factor that significantly strengthens the relevance of the findings.
Also Read: LungVax vaccine: World’s first lung cancer prevention Trial gets £2.06M funding
The Central Role of Brain Energy Failure
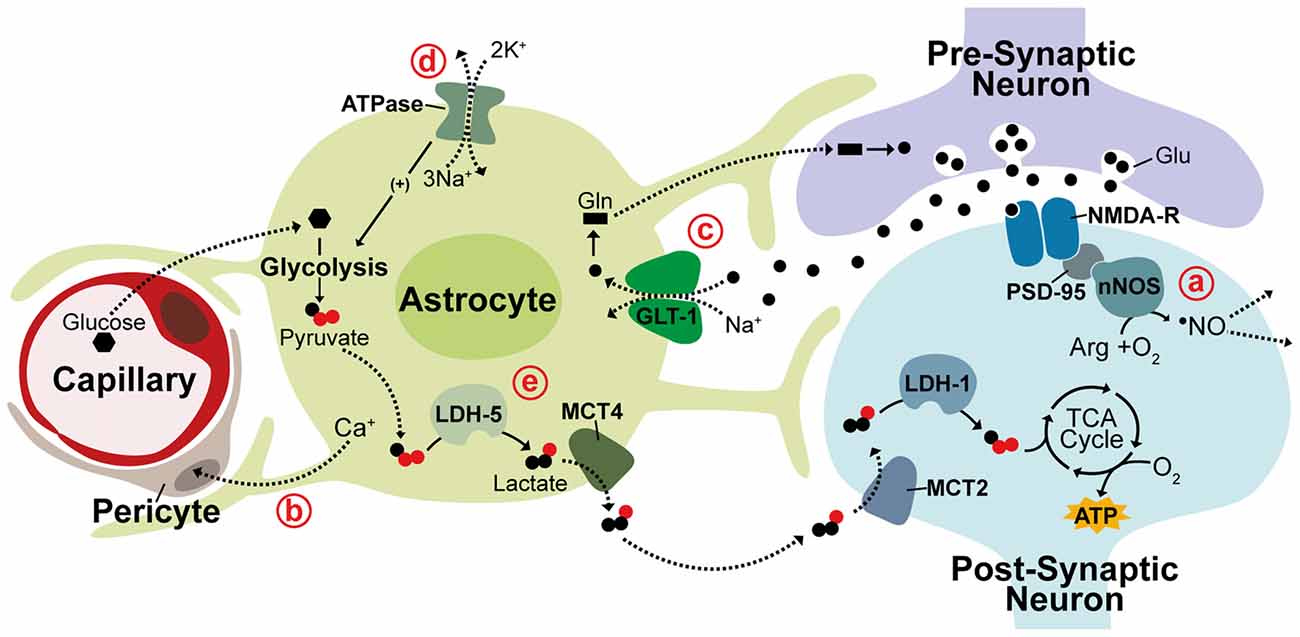
Rather than targeting amyloid plaques or tau tangles directly, the researchers focused on a different biological mechanism: neuronal energy metabolism.
Neurons rely heavily on a molecule called NAD⁺ (nicotinamide adenine dinucleotide) to maintain energy production, repair DNA damage, and protect against cellular stress. Previous research has shown that NAD⁺ levels decline significantly in aging brains and even more sharply in Alzheimer’s disease.
When NAD⁺ levels fall, neurons struggle to maintain normal function, making them vulnerable to degeneration long before structural damage becomes visible.
The researchers hypothesized that restoring this energy balance could reverse downstream effects of the disease.
You may find interesting: Bryan Johnson’s Detox Method: Know How to remove microplastics from semen
How Alzheimer’s Reversal in Mice Was Achieved
To test this hypothesis, scientists administered a compound designed to stabilize NAD⁺ levels and prevent metabolic collapse in neurons.
Following treatment:
- Neuronal energy metabolism returned to near-normal levels
- Synaptic function improved
- Memory performance recovered in behavioral tests
This metabolic intervention led to functional recovery rather than mere symptom suppression, supporting the claim of Alzheimer’s reversal in mice.
Memory Restoration: Evidence from Cognitive Testing
The mice underwent standardized cognitive assessments commonly used in neuroscience research, including maze-based learning and memory recall tests.
Before treatment, Alzheimer’s-affected mice showed clear deficits in spatial memory and learning speed. After metabolic restoration, their performance closely matched that of healthy control animals.
Importantly, these behavioral improvements were not temporary. Memory recovery persisted throughout the observation period, suggesting sustained neurological repair rather than short-term stimulation.
You can read: Natural Relief for Chronic Constipation: Diet Strategies That Work
Biomarker Normalization Strengthens the Findings
In addition to behavioral recovery, researchers observed normalization of several Alzheimer’s-associated biomarkers in blood samples. This included markers linked to tau pathology and neuronal stress.
The alignment of functional improvement with biochemical correction strengthens the conclusion that the disease process itself was modified, rather than masked.
Related: What is Frontotemporal Dementia? Understanding Bruce Willis’ Diagnosis
Why This Study Matters for Alzheimer’s Research
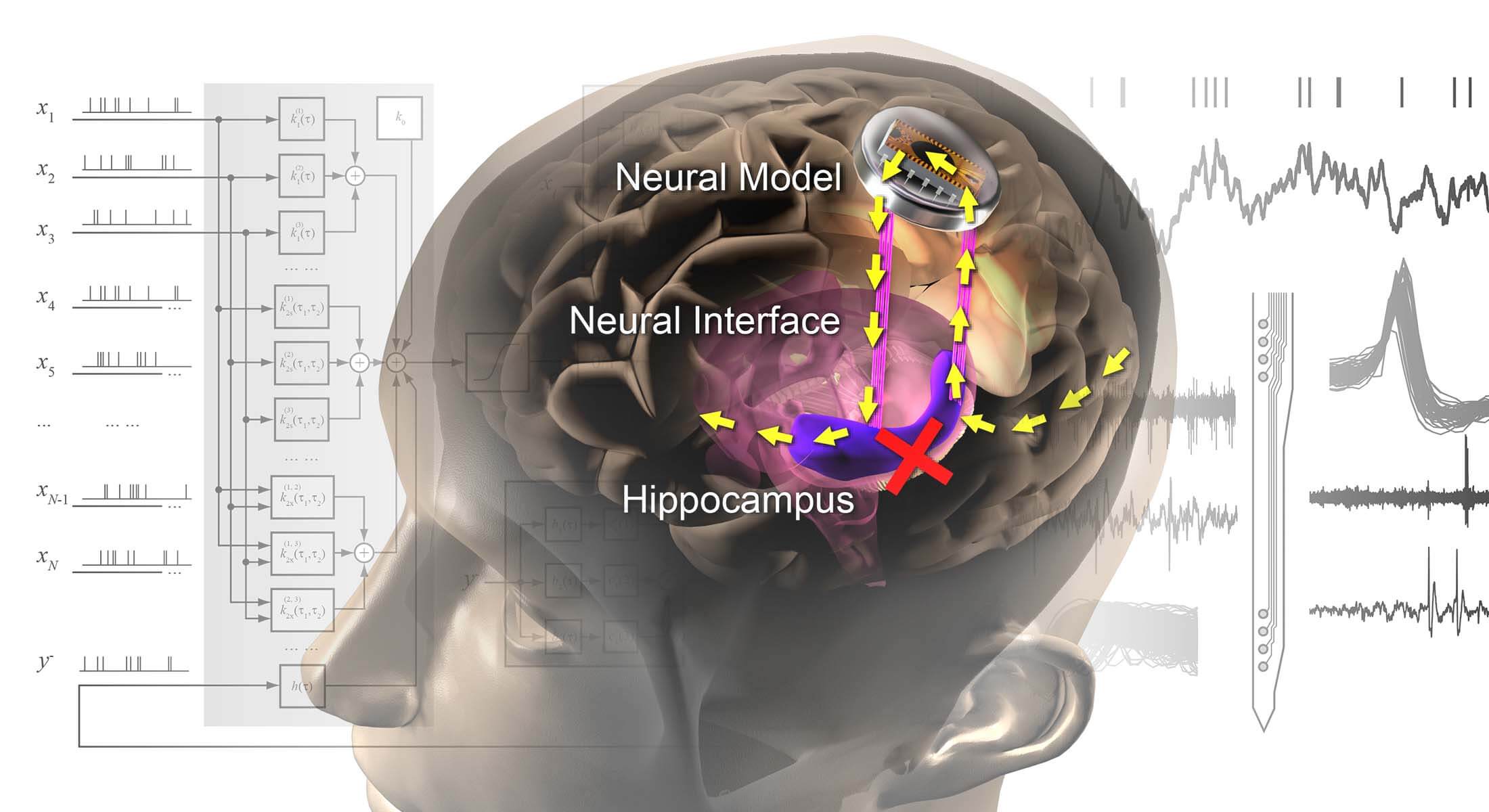
The significance of Alzheimer’s reversal in mice extends beyond a single experimental result. It introduces a conceptual shift in how the disease may be understood and treated.
First, it suggests that neuronal dysfunction may precede irreversible neuronal death and that restoring cellular health could allow recovery. Second, it supports the idea that Alzheimer’s is not solely a protein-aggregation disorder but also a metabolic disease of the brain.
Finally, the effectiveness of treatment after symptom onset is particularly relevant, as most human patients are diagnosed only after noticeable cognitive decline.
Also read: The Cancer Sugar That May Help Cure Type 1 Diabetes
Caution: Translating Mouse Results to Humans
Despite the promising findings, experts emphasize caution. Alzheimer’s disease in humans is biologically more complex than in animal models, involving genetic, vascular, immune, and lifestyle factors that cannot be fully replicated in mice.
Historically, many therapies that succeeded in animal models failed in human clinical trials. Therefore, Alzheimer’s reversal in mice should be interpreted as proof of biological possibility, not immediate clinical applicability.
Human safety studies and controlled trials will be required to determine whether restoring brain energy metabolism can produce similar benefits in patients.
Important medical info: Why Regular Check-ups during Pregnancy Is Essential?
What Happens Next in Research
The next phase of investigation will focus on:
- Assessing safety of metabolic stabilizing compounds in humans
- Identifying optimal treatment timing
- Validating metabolic biomarkers for early diagnosis and response monitoring
- Exploring combination therapies integrating metabolism, inflammation control, and protein clearance
If successful, future Alzheimer’s treatment strategies may focus on maintaining neuronal resilience rather than solely targeting pathological aggregates.
You can read: The Effects of Dehydration on the Human Body: Symptoms, Diseases, Tests, and Prevention
Implications for Patients and Clinicians
For patients and families affected by Alzheimer’s, the study offers cautious optimism rather than immediate solutions. It reinforces the importance of early diagnosis and supports growing interest in brain metabolism as a therapeutic target.
Clinicians and researchers view the findings as an important step toward redefining Alzheimer’s as a potentially modifiable disease process, rather than an inevitably degenerative condition.
Final Perspective
The demonstration of Alzheimer’s reversal in mice represents a meaningful advance in neuroscience, not because it promises an instant cure, but because it reshapes scientific understanding of what may be biologically possible.
By showing that memory loss can be reversed under specific metabolic conditions, the study opens new directions for research that extend beyond symptom management toward genuine disease modification.
Whether this approach can succeed in humans remains to be seen, but the findings mark a critical shift in Alzheimer’s research — from inevitability to possibility.