Heart disease remains the leading cause of death worldwide, with millions of new cases diagnosed each year. In India alone, cardiovascular diseases account for nearly 28% of all deaths. The tragedy lies in the fact that many of these cases could be prevented or managed better with timely detection with proper medical tests to detect heart disease risk.
To stay one step ahead, cardiologists recommend a series of tests, lifestyle changes, and natural remedies that can detect heart disease risk early and improve quality of life. This article explores everything you need to know about heart disease symptoms, initial screenings, advanced tests, treatments, naturopathy options, and caring practices.
Table of Contents
Common Heart Disease Symptoms
Heart disease develops silently in many people, but certain symptoms should never be ignored.
- Chest Pain or Discomfort (Angina) – Pressure, squeezing, or heaviness in the chest.
- Shortness of Breath – Especially during physical activity or while lying flat.
- Palpitations – Rapid or irregular heartbeat.
- Fatigue and Weakness – Persistent tiredness, even after rest.
- Swelling in Legs, Ankles, or Feet – Due to fluid retention (edema).
- Lightheadedness or Fainting – Can indicate arrhythmias or low blood flow.
- Jaw, Neck, or Arm Pain – Radiating pain, often a sign of heart attack.
⚠️ These signs require immediate cardiology evaluation. If severe chest pain or sudden breathlessness occurs, emergency care is critical.
Related: The Effects of Dehydration: Symptoms, Diseases, Tests, & Prevention
Initial Tests to Detect Early Heart Disease

1. Blood Pressure Measurement
What it tests: The force of blood against arterial walls, captured as systolic/diastolic values. Elevated levels often present no symptoms but dramatically increase risks of heart attack, stroke, and cognitive decline. (www.heart.org)
When to start: From age 18.
Frequency: At least every two years if reading is under 120/80 mm Hg; more often if higher or risk factors exist.
2. Lipid Profile (Cholesterol & Triglycerides)
What it reveals: Levels of total cholesterol, LDL (“bad”), HDL (“good”), and triglycerides. Elevated LDL or triglycerides signal heightened risk of arterial plaque buildup.
When to start: Around age 20; earlier if you have a family history or risk factors.
Frequency: Every 4–6 years if normal; men aged 45–65 and women 55–65 should test every 1–2 years; annually over age 65.
3. Blood Glucose Test (Including HbA1C)
What it checks: Fasting glucose or HbA1C levels to detect prediabetes or diabetes — both major risk multipliers for heart disease. (www.heart.org)
When to start: At age 45 for average-risk individuals; earlier if overweight, hypertensive, or with family history.
Frequency: About every three years, unless earlier testing is warranted by risk.
4. BMI & Waist (or Neck) Measurements
Why it matters: Body Mass Index and waist circumference gauge body fat and distribution — central obesity strongly correlates with heart and metabolic risk.
Neck circumference is gaining traction as a quick, predictive marker of cardiometabolic risk.
When to start: From early adulthood, at routine health visits.
5. Heart Risk Calculators (Framingham, ASCVD, PREVENT™)
Purpose: Combine multiple risk factors (age, cholesterol, blood pressure, smoking, diabetes) into a 10-year cardiovascular risk estimate, guiding prevention. (NHLBI, MedlinePlus)
When to start: In your 20s–30s; more comprehensive tools apply up to age 79.
Frequency: Every 4–6 years, or sooner if risk factors change.
6. Coronary Artery Calcium (CAC) Score
What it measures: CT-based assessment of calcified plaque in coronary arteries — a sensitive early sign of atherosclerosis. Higher CAC means higher heart attack risk. (Hopkins Medicine)
When to start: Age 40+ in men, 50+ in women, especially when risk is unclear.
Frequency: Used selectively; not part of routine repeated screening.
7. Inflammatory & Genetic Lipid Markers (hs-CRP, Lp(a), ApoB)
Why they matter: High-sensitivity C-reactive protein signals systemic inflammation; Lp(a) and apolipoprotein B expose genetic cholesterol risk often missed by standard tests. (Health)
When to start: In your 30s–40s if family history or risk ambiguity exists.
Frequency: Typically once, or repeated as indicated.
8. Advanced Biomarkers (Troponin I, Ceramides, BNP)
What’s new: High-sensitivity Troponin I, natriuretic peptides (BNP), and ceramides are emerging as strong predictors of cardiovascular events — even in asymptomatic individuals.
When to use: In higher-risk individuals or models for personalized prevention; clinical discretion applies.
9. Electrocardiogram (ECG/EKG)
What it does: Records heart’s electrical activity — useful for detecting arrhythmia or prior heart damage.
When to start: Not recommended routinely for asymptomatic, low-risk individuals due to false positives and potential harm.
10. Advanced Imaging & Vascular Markers (CIMT, UACR)
Purpose: Carotid Intima-Media Thickness (CIMT) and Urine Albumin-to-Creatinine Ratio (UACR) detect early vascular or kidney damage often preceding clinical disease.
When to use: In people with high risk, hypertension, or unclear screening results.
Related: Why Regular Check-ups during Pregnancy Is Essential?
Why Early, Regular Screening Matters

Cardiovascular disease remains the leading cause of death globally. Screening reduces morbidity and mortality by catching risk early.
A recent update in blood pressure guidelines emphasizes tighter control and earlier intervention. And advances like the PREVENT calculator, stricter hypertension detection, and using UACR for kidney-related risk reflect evolving precision medicine approaches.
Your Heart Health Timeline (Age-Based Guidance)
| Age Group | Recommended Actions |
|---|---|
| 20–30 | Annual BP; lipid every 4–6 years; BMI/waist; risk calculator. |
| 40–50 | Add glucose, hs-CRP/Lp(a)/ApoB; consider CAC (esp. if risk uncertain). |
| 50+ | Annual screening for lipids, glucose; CAC if not done; vascular imaging if needed. |
| High-Risk | Early and frequent tests; advanced biomarkers; specialist follow-up. |
Advanced Tests for Critical Heart Disease Symptoms
When patients show warning signs of heart disease or when initial screenings indicate risk, cardiologists turn to more advanced diagnostic tools. These tests provide detailed insights into heart structure, blood flow, and blockages.
1. Stress Test (Treadmill Test, TMT)
It measures the heart’s performance under physical stress, usually while walking or running on a treadmill with ECG monitoring. It detects reduced blood supply to the heart muscles.
- When to start: For people with chest pain, breathlessness, or suspected coronary artery disease.
- Frequency: As recommended by a cardiologist, not routine for healthy individuals.
2. Holter Monitoring
It’s a 24–48-hour continuous ECG recording to detect irregular heartbeats (arrhythmias) that may not show up in a standard ECG.
- When to start: If patients report palpitations, dizziness, or unexplained fainting.
- Frequency: Ordered only when symptoms are present.
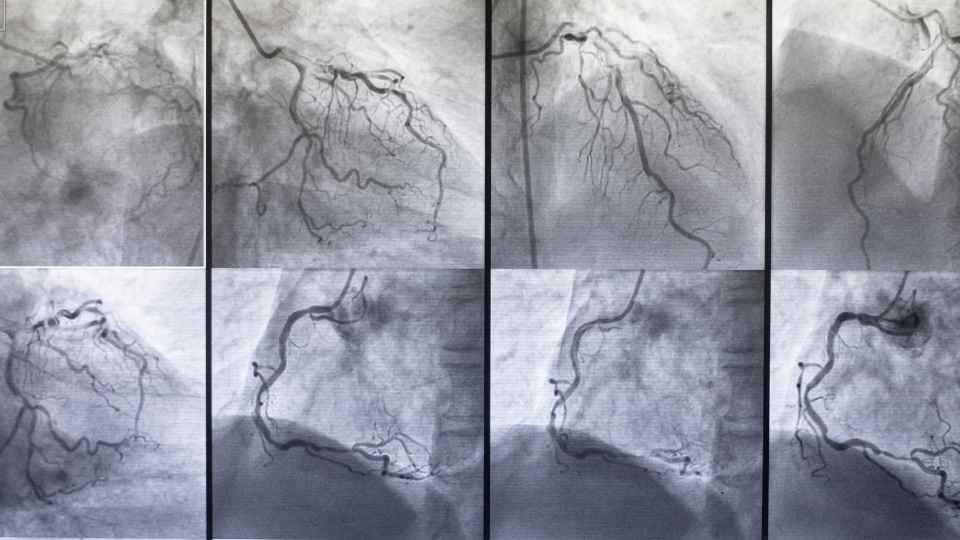
3. Coronary Angiography
It’s an invasive imaging test using a catheter and dye to visualize blocked or narrowed coronary arteries. Considered the gold standard for diagnosing coronary artery disease.
- When to start: If severe symptoms, high-risk stress test results, or heart attack suspicion.
- Frequency: Performed only when strongly indicated; not for general screening.
4. Cardiac CT / MRI
It measures advanced imaging that visualizes the heart’s anatomy, function, and blood vessels. CT angiography identifies blockages; MRI evaluates tissue damage (e.g., after a heart attack).
- When to start: If non-invasive tests are inconclusive or when a detailed heart structure assessment is needed.
- Frequency: Case-specific, guided by cardiologist.
5. Troponin Blood Test
It measures Levels of cardiac enzymes (troponins) released into the blood during heart muscle damage. Critical for diagnosing heart attacks.
- When to start: In emergency settings (chest pain, suspected heart attack).
- Frequency: Only during suspected acute events, not for routine use.
Career in Health: Join Government-Approved Paramedical DRD Course Under WBSMF
Treatment Options for Heart Disease
If tests confirm heart disease, treatment depends on severity. Cardiologists usually combine medications, lifestyle modification, and sometimes surgery.
1. Medications
- Statins (cholesterol control)
- Beta-blockers (reduce BP and heart strain)
- ACE inhibitors/ARBs (manage BP and protect heart function)
- Antiplatelet drugs (aspirin, clopidogrel — reduce clot formation)

2. Surgical & Interventional Procedures
- Angioplasty & Stent Placement: Opens blocked arteries.
- Bypass Surgery (CABG): Reroutes blood flow around severe blockages.
- Pacemakers / ICDs: Control rhythm disturbances.
3. Lifestyle Interventions
- Quitting smoking and alcohol reduction
- Healthy weight management
- Structured exercise plan under medical supervision
Health News for You: What is Frontotemporal Dementia? Understanding Bruce Willis’ Diagnosis
Natural Remedies to Keep the Heart Safe
Natural remedies are not just alternatives; they form the foundation of long-term cardiovascular health. The heart thrives when supported by simple but consistent lifestyle practices.
A balanced diet rich in vegetables, fruits, legumes, nuts, whole grains, and healthy fats like olive oil reduces cholesterol and inflammation. Omega-3 sources such as fish, walnuts, and flaxseeds protect arteries and lower arrhythmia risk.
Regular exercise — brisk walking, swimming, or cycling — strengthens the heart muscle, improves circulation, and keeps blood pressure stable. Just 30 minutes a day can cut the risk of heart disease significantly.
Stress management is equally crucial. Yoga, meditation, and deep breathing lower cortisol and prevent chronic strain on the heart. Adequate sleep and hydration further support heart function by stabilizing hormones and reducing blood viscosity.
Together, these natural strategies create a protective shield for the heart, delaying disease onset and improving quality of life.
Health Awareness: Microplastics in Human Reproductive Fluids: A 2025 Wake‑Up Call for Fertility
Naturopathy Options for Heart Disease
Naturopathy views the human body as a self-healing system that thrives when given the right conditions. For heart disease management, naturopathy does not aim to replace modern cardiology but to complement it with supportive therapies that improve quality of life and reduce dependency on heavy medication where possible.
Herbal remedies like Terminalia arjuna strengthen cardiac muscles, garlic helps lower cholesterol, and turmeric reduces inflammation. Green tea improves vascular flexibility through antioxidants.
Hydrotherapy (alternating hot-and-cold baths or warm immersion) stimulates circulation and relaxes blood vessels, beneficial for mild hypertension. Massage with essential oils such as lavender or sandalwood calms the nervous system and lowers stress-induced palpitations.
Dietary naturopathy emphasizes plant-based detox diets, rich in sprouts, raw vegetables, and herbal teas, to boost antioxidant intake and regulate cholesterol.
Each remedy targets a specific need — arjuna for strength, garlic for lipid control, hydrotherapy for circulation, meditation for stress. Used under professional guidance, naturopathy enhances healing and supports long-term heart care.
Health News: What is Lyme Disease? The Illness That Justin Timberlake Was Diagnosed With
Caring for Heart Patients: Beyond Treatment
Living with heart disease requires holistic support. Families and caregivers play an essential role.
- Dietary supervision: Prepare heart-friendly meals.
- Medication adherence: Ensure doses are taken on time.
- Naturopathy: Get help from a certified Naturopath for quick healing & reduce long-term medication.
- Emotional support: Depression is common in cardiac patients; counseling helps.
- Regular monitoring: BP, sugar, and cholesterol checks at home.
- Rehabilitation programs: Cardiac rehab improves recovery after surgery or heart attack.
Health Science Discovery: Cancer Sugar May Help Cure Type 1 Diabetes
Conclusion: Proactive Heart Care is Lifelong Care
Heart disease is not a sudden event but a condition that develops silently over the years. Recognizing early symptoms, undergoing routine and advanced tests at the right time, following treatment plans, and adopting natural + holistic care can save lives.
As cardiologists emphasize: The earlier the detection, the better the outcome. Prevention, awareness, and lifestyle choices remain the strongest weapons against heart disease.
So, if you feel things are not right, talk with your doctor to create a personalized screening plan. Your heart powers more than your emotions — it powers your life. Don’t wait until it’s too late.